MEDICAL
Bariatrics
Enhance the success of weight management programs.
Enhance the success of weight management programs.
Body composition is essential for understanding the patient’s physiological makeup and guiding targeted therapies to enhance the success of weight management programs. InBody devices are non-invasive and convenient, making it the ideal tool to implement into clinical practice. The InBody test provides comprehensive results that can be used to educate and engage the patient as well as track health improvements throughout patient interventions.
In less than 60 seconds, the InBody test provides easy-to-understand, accurate and objective measurements to evaluate health risks and monitor progress. Bariatric professionals can use the InBody to:
“…minimizing lean mass loss is an important health and safety consideration in order to maintain strength and physical function and also to maximize basal metabolic rate for long-term weight maintenance.”
“…percentage body fat has been recommended for use in epidemiologic research on adiposity rather than BMI and other anthropometric measures.”
“Body composition measurements can provide information on fat, muscle content, and basal metabolic rate, which can be used for weight loss programs and follow-ups.”
Current methods for body weight assessment do not provide insight into the physiological makeup of the patient, which may limit tailoring treatments and interventions. Body composition allows bariatric specialists to create targeted treatment plans for each individual patient.
By assessing the balance between muscle and fat composition allows specialists to identify cardiometabolic risks more appropriately as well as identify those who carry an imbalance in muscle and fat mass. Patients with low muscle mass in conjunction with excess fat mass (sarcopenic obesity) are at increased health risks and require different diet and exercise programs to prevent loss of muscle and improve functional status.
The distribution of fat mass also impacts health risk – Segmental Fat Analysis provides a better overall insight into fat distribution. Visceral Fat Area provides an indication of the fat most associated with cardiometabolic health risks, affording more precise tools for identification of risk of diabetes, cardiovascular disease, etc.
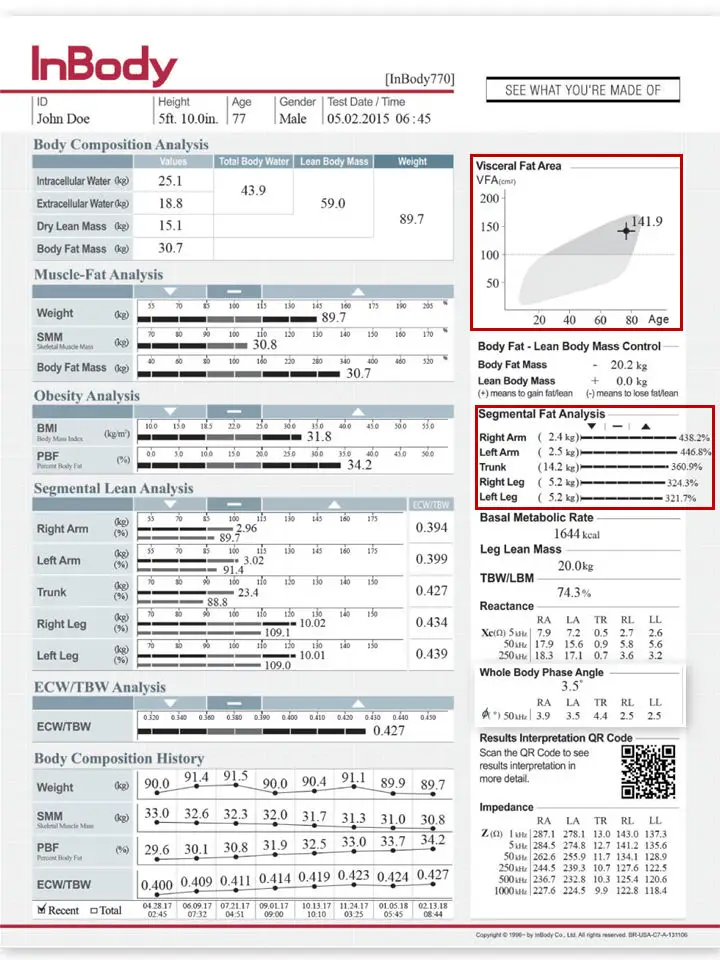

Obesity accompanied by low levels of lean mass, particularly in the legs, can increase risk of falls that can result in frailty, limited functional capacity, and/or reduced quality of life. Segmental measures allow for precise analysis of lean body mass distribution to help the clinician assess risks associated with reduced lean mass.
The Segmental Lean Analysis (SLA) section can quickly assess a patient’s frailty status and functional mobility risk. By segmenting the body, areas of low lean mass can be identified and targeted for improvement, helping reduce risk of falls and/or injuries. The top bar of the SLA provides an objective measure of lean body mass, while the bottom bar incorporates an in-depth analysis into:
Identifying areas of low lean mass can help tailor more specific programs to improve patient outcomes such as functional status and quality of life both before and after bariatric surgery. By correcting areas of weakness this will not only help the patient’s health but improve lifestyle as well.
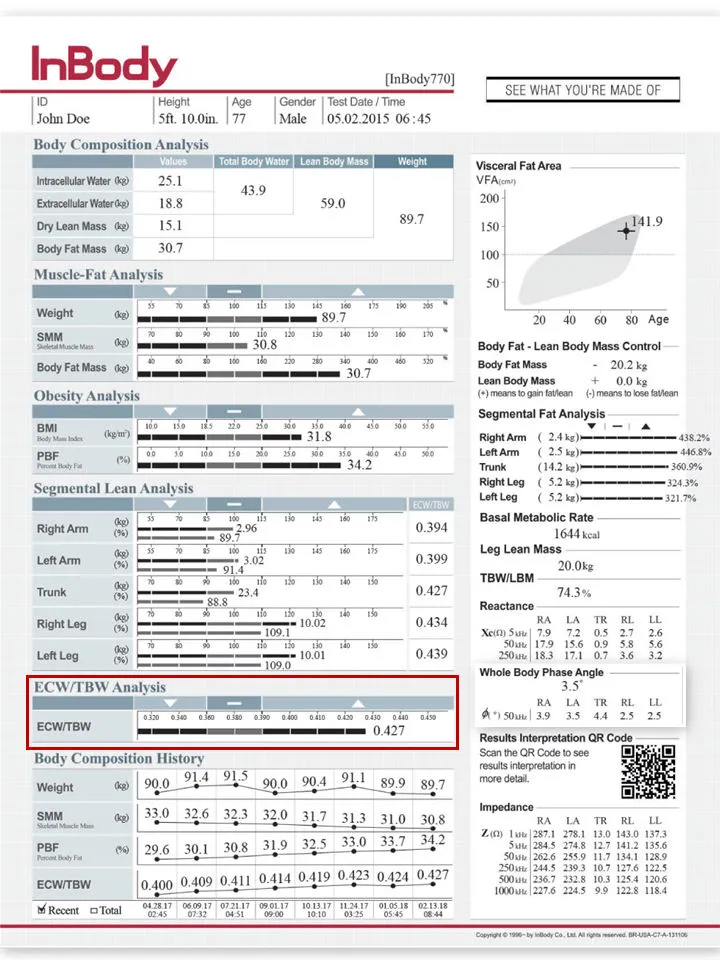
Obesity is often accompanied by hormonal and other physiological changes resulting in inflammation or fluid retention (edema). However, current diagnostic markers of fluid balance are imprecise and time-consuming. InBody provides objective measures for monitoring whole-body and segmental fluid balance.
InBody effectively distinguishes water in the intracellular (ICW; within the tissues) and extracellular (ECW; within the blood and interstitial fluids) compartments that make up total body water (TBW). The Edema Index, based on the ratio between ECW and TBW (ECW/TBW), can be used to detect fluid imbalances resulting from systemic inflammation that is commonly associated with obesity.
Furthermore, it can be used to track changes in fluid balance and improvements in patients post-surgery. Additionally, this marker can help identify sustained inflammation linked to circulation issues or post-surgical complications. Evaluating ECW/TBW, physicians have the ability to identify changes in weight resulting from changes in body composition and/or fluid imbalance; this ability to track changes precisely allows for improved health outcomes for each individual patient.

Weight and BMI are not appropriate measures to track health improvements through interventions. Rather than simple weight loss, track changes in body composition for a more comprehensive analysis of health improvement.
Weight loss or changes in BMI do not capture the composition of weight lost. With simple weight reduction, patients tend to lose muscle or excess water along with fat mass. In order to ensure proper weight loss and improvements in long-term health, tracking changes in muscle, percent body fat, and fluid balance key for adjusting/developing customized treatments. Changes in muscle-fat balance as well as lean and fat mass distribution can also be tracked from test to test in the Body Composition History section to confirm patient progress with exercise, diet, or drug therapies as well as surgical interventions. With a comprehensive assessment of body composition, bariatric specialists will be able to educate and set treatment plans with each patient to produce better motivation and success.
All InBody professional body composition analysers rely on four pillars of technology to deliver quick, accurate and precise results. These pillars allow you to trust that the results reflect your patients’ true health from the inside out.
DIRECT SEGMENTAL MEASUREMENT (DSM)
Direct Segmental Measurement (DSM) measures water, muscle mass and fat mass in the five body segments: right arm, left arm, left leg, right leg and trunk. By measuring each segment of the body separately, the InBody provides an in-depth analysis of the patient’s muscle-fat and fluid balance in each segment independently. Identifying the patient’s msucle and fat distribution allows a better assessment of associated health risks, and segmental ECW/TBW can be used to identify systemic or localized inflammation resulting from obesity and underlying health conditions or surgical intervention. With a comprehensive analysis of each part of the body, bariatric physicians will be better equipped to address each patient’s unique concerns and create targeted health plans to enhance patient success.
MULTIPLE FREQUENCIES
InBody devices utilize multiple frequencies to measure body water more accurately than commonly-used methods such as weight changes or pitting edema scores. These high and low frequencies measure both intracellular and extracellular water, producing precise measures of body water compartments. With accurate fluid measures, InBody can be used to identify fluid imbalances or water retention stemming from inflammation or circulation issues as well as monitor changes in fluid balance resulting from surgical or treatment interventions.
8 POINT TACTILE ELECTRODES
InBody devices use an 8-Point Tactile Electrode system to ensure that measurements always start in the same place, test after test. This technology creates precise and reproducible results, ensuring that the results obtained are a direct outcome of clinical recommendations and interventions, rather than error.
NO EMPIRICAL ESTIMATIONS
InBody devices do not rely on empirical estimations based on age, gender or ethnicity to predict results. With the high level of accuracy and precision achieved with aforementioned technological advancements, InBody removes population-associated assumptions when determining body composition to ensure that results are solely based on the individual and increasing sensitivity to body composition changes.